How does diabetes affect the retina?
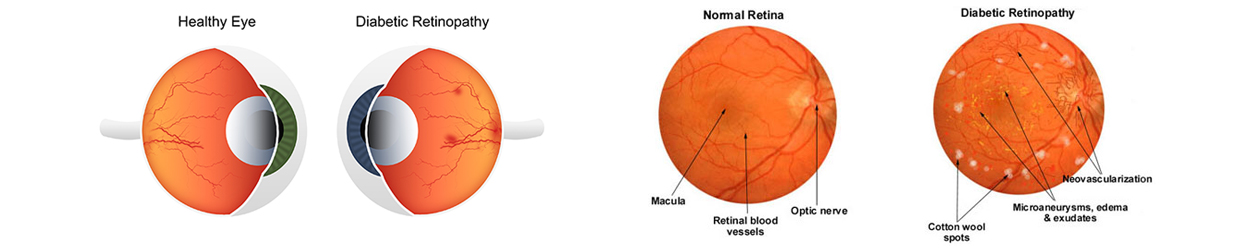
- Diabetic retinopathy is a major cause of blindness. There are two major types of diabetic retinopathy.
- One form (proliferative retinopathy) is characterized by the growth of new blood vessels on the surface of the retina, which may lead to hemorrhage and scarring of the retina.
- A second form, edematous or background retinopathy is characterized by leakage of small blood vessels in the retina, which causes reduced vision.
How can I know the extent of diabetic damage to my retina?
- People with diabetic retinopathy may not suffer reduced vision in the early stages, and therefore, regular eye examinations by an ophthalmologist are important, especially for people who have been diabetic for a number of years.
- A detailed fundus examination every year is a must for every diabetic patient.
How potentially blinding diabetes can be?
- Retinal changes are the major problem
- At times diabetes can also cause a rise in
- eye pressure (glaucoma)
- clouding of the lens (cataract)
- weakness of the optic nerve or eye muscle.
- Cataracts often occur at a younger age in diabetic patients.
- Glaucoma can cause damage to the optic nerve. In fact diabetes is one of the several possible causes of glaucoma.
- Damage to the small vessels of the optic nerve can affect vision, and weakness of the eye muscles may cause double vision.
- A diabetic is also more likely to develop sudden vision loss due to occlusion of the retinal vessels (branch or central retinal vein occlusion), bleeding in the vitreous cavity, detachment of the retina, or infections of the cornea and vitreous.
How is diabetic retinopathy treated?
- The indications for treatment depend on extent of severity of the disease.
- Laser is the only effective treatment for the proliferations in diabetic eyes.
- If only the central seeing area is affected then usually one sitting of Laser treatment suffices.
- If there are new blood vessels growing, then the eye is divided into four quadrants and a complete PRP i.e. four sittings of Laser are done spanning over a week to ten days.
What is the treatment technique?
- The aim of treatment by laser photocoagulation is to induce involution of new vessels and prevent recurrent vitreous haemorrhage.
- Initial treatment involves the placement of about 2000 – 3000 burns in scatter pattern, extending from the posterior fundus to cover the peripheral retina in one or more sessions.
- Follow-up is done after an interval of 4-8 weeks.
- Treatment of recurrence is done by further Argon Laser PRP filling in any gaps between previous laser scars.
- The most important cause of persistent neovascularization is inadequate treatment. In most eyes, once retinopathy is quiescent, stable vision is maintained.
What are the complications of Laser treatment?
- Laser treatment can cause an initial blurring of vision for the first 4-6 weeks. The vision usually becomes stable after that.
- Major complications like vitreous haemorrahge and detachment are rarely seen.
It is now possible to directly visualize Retinal Layers with OCT
Our centre is equipped with an OCT with the help of which:
- Structures of the Retinal Layers are now directly visible and measurable.
- Macular thickness in diabetic macular edema is quantified; intraretinal or subretinal fluid accumulation can be tracked.
- Post treatment resolution of retinal thickening can be monitored.
